A strong utilization review nurse resume is essential if you’re aiming to land a role in case management, insurance, or healthcare systems that rely on accurate care evaluations.
Your job involves assessing the necessity and efficiency of medical services, which requires a unique blend of clinical knowledge and administrative precision.
In this guide, we’ll walk you through how to write a resume online to highlight your skills, structure your experience, and present yourself as the ideal candidate for this specialized position.
Utilization review nurse resume examples
- Prospective utilization review nurse resume
- Concurrent utilization review nurse resume
- Retrospective utilization review nurse resume
Prospective utilization review nurse resume sample
Prospective utilization review nurse resume template
Resume for prospective utilization review nurse | Plain text
Jennifer Green
Houston, TX | (123) 456-7890 | jgreen@email.comSummary
Detail-oriented and compassionate Prospective Utilization Review Nurse with experience in assessing medical necessity for pre-authorization processes. Skilled in analyzing treatment plans, ensuring compliance with healthcare policies, and facilitating efficient care delivery. Adept at working with physicians, insurance providers, and healthcare teams to improve patient outcomes and minimize costs.
Skills
- Medical necessity review
- Pre-authorization assessments
- Insurance verification
- Clinical documentation
- Patient care coordination
- Case management
- Health policy compliance
- Interdisciplinary communication
- Knowledge of clinical guidelines
- Critical thinking
- Data entry & analysis
- Utilization management software (e.g., Optum, InterQual)
Experience
Prospective Utilization Review Nurse
UnitedHealthcare | Houston, TX | June 2020 – Present
- Review pre-authorization requests for medical procedures and treatments, ensuring they meet clinical guidelines and insurance requirements.
- Collaborate with healthcare providers to clarify treatment plans and provide recommendations for alternative therapies when necessary.
- Utilize clinical decision-making tools such as InterQual and MCG to assess the appropriateness of requested procedures.
- Achieve a 15% reduction in approval turnaround time by streamlining communication with healthcare providers.
- Provide educational support to physicians and healthcare teams about insurance policy requirements and pre-authorization processes.
Registered Nurse
Memorial Hermann Health System | Houston, TX | May 2017 – May 2020
- Delivered patient care in a fast-paced emergency department, coordinating with physicians and specialists.
- Assessed patient health conditions, ensuring accurate documentation and implementation of treatment plans.
- Assisted with patient admissions, discharge planning, and post-operative care.
- Trained new nursing staff on patient care protocols and safety guidelines.
Education
Bachelor of Science in Nursing (BSN)
University of Houston, TX | Graduated: May 2017Certifications
- Registered Nurse (RN) – Texas Board of Nursing, License #123456
- Certification in Utilization Review (CUR) – American Nurses Credentialing Center (ANCC), 2021
Professional Development
- Ongoing training in InterQual Clinical Decision Support System
- Completed 20 hours of continuing education in Medical Coding and Billing, 2023
- Attended the Healthcare Utilization Management Conference, 2022
Strong sides of this utilization review nurse resume example:
- Clear focus on pre-authorization processes and clinical decision-making tools, showcasing expertise in prospective review.
- Demonstrates quantifiable achievements, such as a 15% reduction in approval turnaround time, adding measurable value.
- Professional development section highlights continuous learning, emphasizing up-to-date skills and industry engagement.
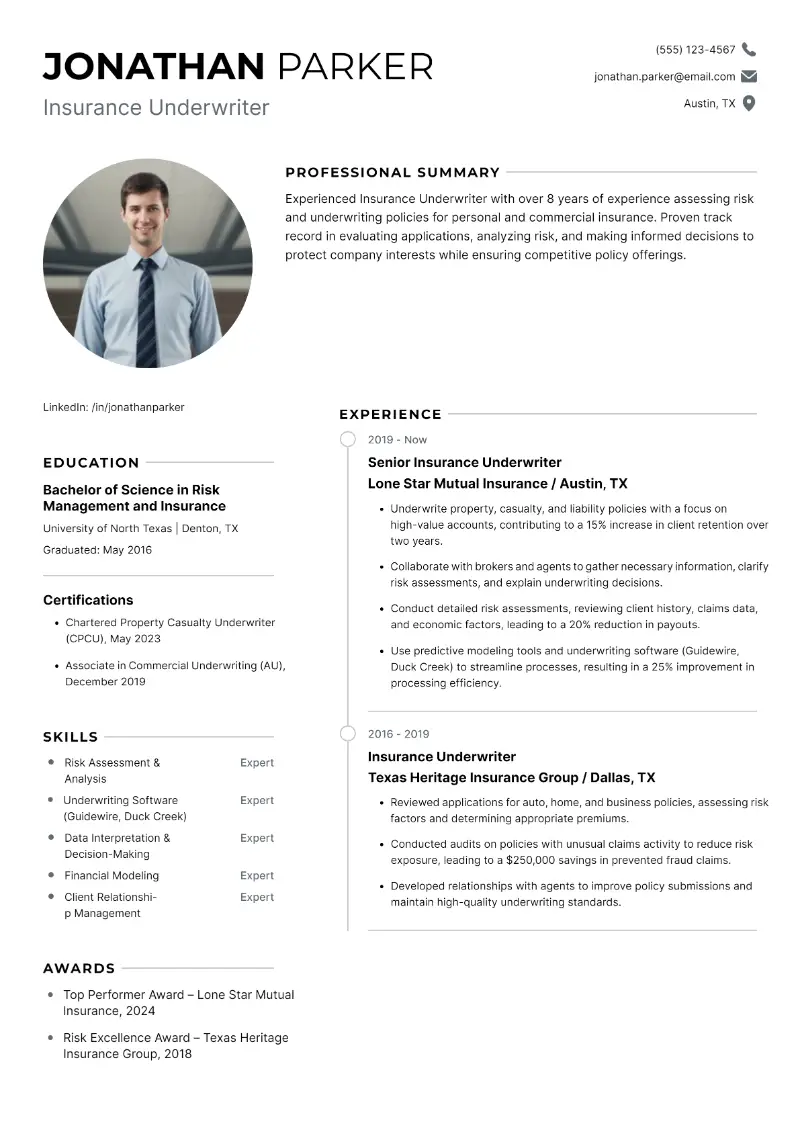
- How to properly format a resume for a utilization review nurse?
- Stick with classic fonts like Arial, Calibri, or Times New Roman in size 10-12 for easy readability.
- If you have several years of experience, limit the resume length to two pages. For entry-level nurses, one page is usually enough.
- 1 inch is the standard margin size, ensuring your document doesn’t look too crowded or too empty.
- Use single spacing so that all the important information fits on the page neatly.
- It’s important to separate resume sections clearly, such as between your summary, skills, experience, and education.
- Left alignment is the most natural format, helping your application maintain structure.
- Stick with black text on white or light-colored paper. Any additional colors or images can be seen unprofessional.
To avoid formatting problems and having to rewrite your paper from scratch try an resume builder for free.
Resume Trick provides modern resume templates that save you time and ensuring that your draft looks polished. They come with AI suggestions for some sections to help guide your content.
Create your professional Resume in 10 minutes for FREE
Build My Resume
Concurrent utilization review nurse resume example
Sample concurrent utilization review nurse resume
Michael Thompson
Austin, TX | (512) 234-5678 | mthompson@email.comSummary
Experienced Concurrent Utilization Review Nurse with over 11 years in assessing and monitoring ongoing patient care to ensure it aligns with clinical guidelines. Skilled in collaborating with medical teams to make real-time decisions, reviewing treatment plans, and optimizing care delivery for better patient outcomes and cost control.
Skills
- Concurrent utilization review
- Real-time case management
- Interdisciplinary communication
- Utilization review software (e.g., Cerner, Epic)
- Patient assessment
- Care coordination
- Clinical guideline adherence
- Insurance knowledge
- Medical record review
- Critical thinking and decision-making
- Quality improvement initiatives
- Cost control strategies
Experience
Concurrent Utilization Review Nurse
Blue Cross Blue Shield of Texas | Austin, TX | August 2018 – Present
- Review inpatient and outpatient treatments in real-time to determine medical necessity and appropriateness of care.
- Work closely with physicians and case managers to ensure patient care is aligned with both clinical guidelines and insurance policies.
- Improve hospital length-of-stay metrics by recommending alternative care paths for patients with extended stays.
- Conduct regular reviews of patient records and collaborate with healthcare teams to adjust treatment plans as needed.
- Reduced unnecessary treatment costs by 10% through more accurate assessments and early intervention in care decisions.
Registered Nurse (RN)
St. David's Medical Center | Austin, TX | June 2014 – July 2018
- Provided direct patient care in the ICU and general medical-surgical floors, ensuring adherence to patient safety and clinical protocols.
- Assisted with care planning and discharge planning, collaborating with a multidisciplinary team.
- Supported physicians in implementing appropriate treatment plans and monitoring patient recovery.
- Educated patients and families on post-discharge care instructions and health maintenance.
Education
Bachelor of Science in Nursing (BSN)
University of Texas at Austin, TX | Graduated: May 2014Certifications
- Registered Nurse (RN) – Texas Board of Nursing, License #789012
- Certified Case Manager (CCM) – Commission for Case Manager Certification, 2019
- Certification in Concurrent Utilization Review (CUR) – American Nurses Credentialing Center (ANCC), 2019
Achievements
- Awarded "Nurse of the Quarter" for outstanding performance in concurrent reviews and cost-saving initiatives, 2021
- Successfully managed concurrent reviews for over 200 cases monthly, maintaining a 98% accuracy rate in medical necessity determination
- Assisted in streamlining review processes, reducing average case turnaround time by 20%
This utilization review nurse resume example will impress the HRs:
- Strong emphasis on real-time case management, reflecting expertise in concurrent review and urgent decision-making.
- Achievement-oriented, with specific results like a 10% reduction in unnecessary treatment costs.
- Detailed, measurable accomplishments such as managing 200+ cases monthly with 98% accuracy, underscoring reliability and effectiveness.
- Should I choose a utilization review nurse resume objective or summary?
Resume summary is ideal for seasoned nurses or those who want to showcase their achievements.
What it must include:
- Total years of experience
- Key accomplishments or areas of expertise (e.g., clinical skills, leadership, patient care)
- Specialization in utilization review and case management
Utilization review nurse resume summary sample:
Experienced utilization review nurse with 5+ years in case management, specializing in patient care optimization and compliance with healthcare standards. Strong analytical skills in evaluating treatment plans, reducing healthcare costs, and improving patient outcomes.
Resume objective is more suitable for entry-level specialists or those switching careers.
What it must include:
- Your professional goal or aspiration
- How you aim to contribute to the role
Utilization review nurse resume objective example:
A highly motivated registered nurse seeking to transition into a utilization review position to leverage clinical experience in improving patient care and reducing unnecessary medical costs.
- How to showcase your utilization review nurse resume skills?
Employers want to see that you have the right set of skills to succeed in this position.
- Hard skills are technical, job-specific abilities that can be learned through education, training, or practice. For utilization review nurses, this includes medical knowledge, software proficiency, and case management expertise.
- Soft skills are interpersonal traits or qualities that help you interact effectively with others. These are crucial in healthcare settings where communication, teamwork, and problem-solving are key to delivering quality patient care.
Utilization review nurse hard skills:
- Case management
- Medical coding and billing
- Knowledge of insurance policies
- Treatment protocols
- Risk management
- Clinical documentation
- Utilization review
- Patient assessments
- Healthcare quality standards
- Patient advocacy
- Compliance with healthcare laws
- Decision-making
- Cost management
- Knowledge of clinical software (e.g., Epic, Cerner)
- Data analysis
Soft skills for utilization review nurse:
- Communication
- Critical thinking
- Problem-solving
- Attention to detail
- Empathy
- Active listening
- Teamwork
- Organizational skills
- Time management
- Adaptability
- Conflict resolution
- Patient-centered care
- Negotiation
- Decision-making under pressure
- Multitasking
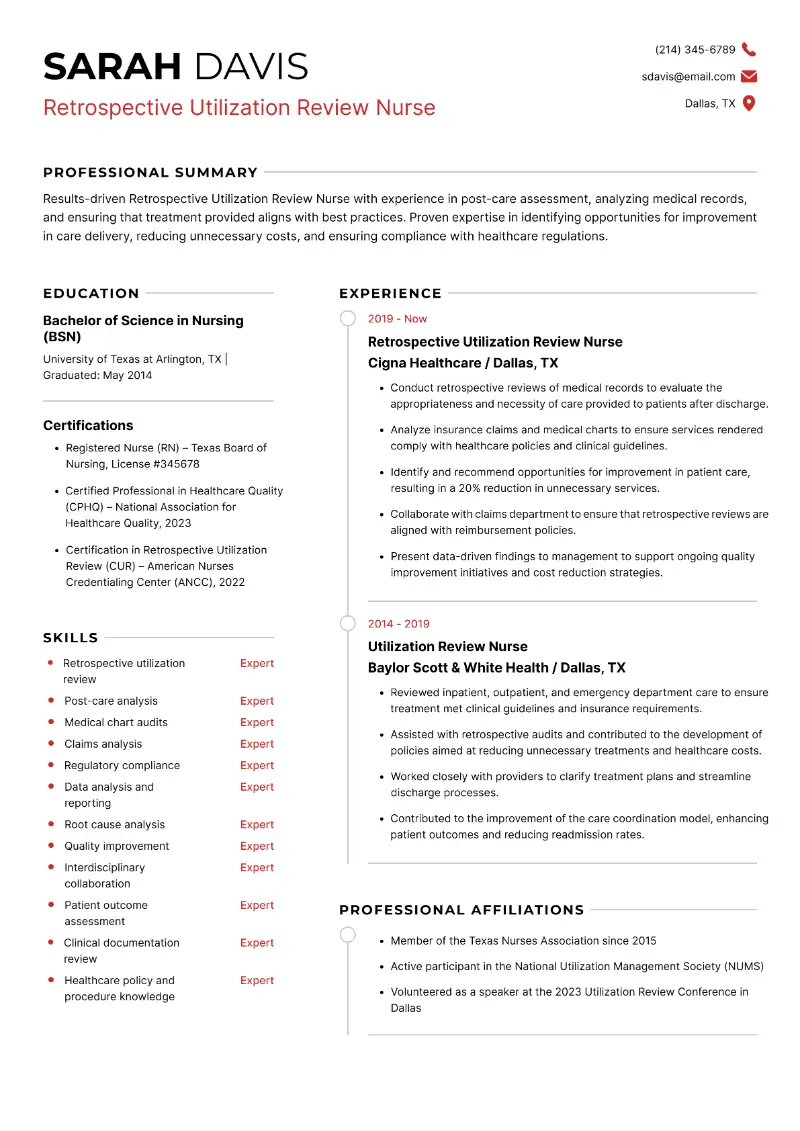
Retrospective utilization review nurse resume template
Retrospective utilization review nurse resume sample
Resume for retrospective utilization review nurse | Text version
Sarah Davis
Dallas, TX | (214) 345-6789 | sdavis@email.comSummary
Results-driven Retrospective Utilization Review Nurse with experience in post-care assessment, analyzing medical records, and ensuring that treatment provided aligns with best practices. Proven expertise in identifying opportunities for improvement in care delivery, reducing unnecessary costs, and ensuring compliance with healthcare regulations.
Skills
- Retrospective utilization review
- Post-care analysis
- Medical chart audits
- Claims analysis
- Regulatory compliance
- Data analysis and reporting
- Root cause analysis
- Quality improvement
- Interdisciplinary collaboration
- Patient outcome assessment
- Clinical documentation review
- Healthcare policy and procedure knowledge
Experience
Retrospective Utilization Review Nurse
Cigna Healthcare | Dallas, TX | March 2019 – Present
- Conduct retrospective reviews of medical records to evaluate the appropriateness and necessity of care provided to patients after discharge.
- Analyze insurance claims and medical charts to ensure services rendered comply with healthcare policies and clinical guidelines.
- Identify and recommend opportunities for improvement in patient care, resulting in a 20% reduction in unnecessary services.
- Collaborate with claims department to ensure that retrospective reviews are aligned with reimbursement policies.
- Present data-driven findings to management to support ongoing quality improvement initiatives and cost reduction strategies.
Utilization Review Nurse
Baylor Scott & White Health | Dallas, TX | June 2014 – February 2019
- Reviewed inpatient, outpatient, and emergency department care to ensure treatment met clinical guidelines and insurance requirements.
- Assisted with retrospective audits and contributed to the development of policies aimed at reducing unnecessary treatments and healthcare costs.
- Worked closely with providers to clarify treatment plans and streamline discharge processes.
- Contributed to the improvement of the care coordination model, enhancing patient outcomes and reducing readmission rates.
Education
Bachelor of Science in Nursing (BSN)
University of Texas at Arlington, TX | Graduated: May 2014Certifications
- Registered Nurse (RN) – Texas Board of Nursing, License #345678
- Certified Professional in Healthcare Quality (CPHQ) – National Association for Healthcare Quality, 2023
- Certification in Retrospective Utilization Review (CUR) – American Nurses Credentialing Center (ANCC), 2022
Professional Affiliations
- Member of the Texas Nurses Association since 2015
- Active participant in the National Utilization Management Society (NUMS)
- Volunteered as a speaker at the 2023 Utilization Review Conference in Dallas
This sample utilization review nurse resume is effective for several reasons:
- Focuses on retrospective review, showing in-depth expertise in post-care assessment and medical chart audits.
- Data-driven with emphasis on cost reduction and quality improvement, appealing to organizations focused on efficiency.
- Professional affiliations and volunteer experience reflect active industry involvement and a commitment to professional growth.
- What academic credentials should I add to my utilization review nurse resume?
The education resume section establishes your qualifications, showing that you have the necessary training to be a nurse.
- Most utilization review nurses hold an RN (Registered Nurse) diploma, but having a BSN (Bachelor of Science in Nursing) or higher is often preferred.
- Include the name of the school where you obtained your degree and its location.
- Add the month and year of graduation. If you have relevant coursework, feel free to mention it here.
- How to organize the experience section in a utilization review nurse resume?
- Always list your work history in reverse chronological order, starting with your current or most recent role.
- Bullet points make your responsibilities and achievements more readable.
- Whenever possible, use numbers to show your impact (e.g., “Reduced treatment approval times by 20%” or “Managed a caseload of 50+ patients per month”).
- Don’t just write job duties. Showcase how your work made a difference in patient outcomes or cost savings.
Conclusion
Your resume is more than just a summary of your work history—it’s a chance to show potential employers that you understand the complexities of utilization review and can contribute to better, efficient healthcare.
By tailoring your document to focus on outcomes, collaboration, and your analytical skills, you can set yourself apart in a competitive job market.
Take the time to refine each section, and you’ll be one step closer to landing your next role as a utilization review nurse.
Create your professional Resume in 10 minutes for FREE
Build My Resume